Suppose the skin on your residual limb had the same thickness, toughness, and pressure resistance as the soles of your feet. You’d probably have fewer rashes, blisters, and sores, no? According to a new study in the journal Science, that kind of transformation might be possible within a few years. Researchers at Johns Hopkins University have successfully tested a cell therapy to increase regular skin’s weight-bearing capacity—and they’re seeking amputee volunteers to test and refine the method. (If you’re interested, here’s how to get in touch—but be advised that you’ll need to be in Baltimore routinely in order to participate.)
The Science study tested whether residual-limb skin could be endowed with the characteristics of volar skin—ie, the type of skin you have on your soles and the palms of your hands. Volar skin is thicker, denser, and more responsive to pressure than nonvolar skin. At a cellular level, volar skin has larger epidermal cells (aka keratinocytes), longer collagen fibers, higher elastin levels, and higher concentrations of a handful of key proteins.
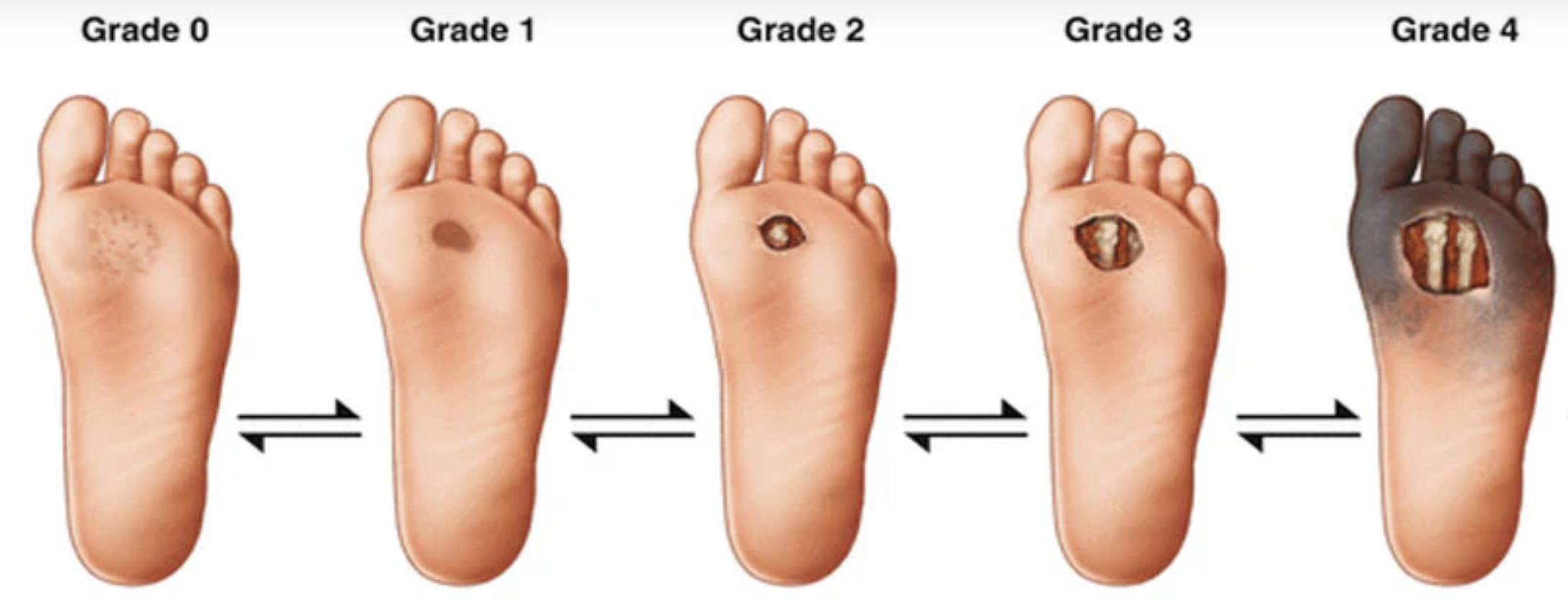
“Our feet bear our weight every day, and the amount of force is incredible,” says Luis Garza, a professor of dermatology at Johns Hopkins and the study’s primary author. “When you run, for example, your feet are bearing enormous amounts of force. So it’s very likely that the cells in that part of our body have become evolutionarily adapted to react to pressure better.” For amputees, that same pressure falls on the residual limb’s nonvolar skin, which isn’t designed to bear weight and withstand high forces.
To test whether cellular therapy could toughen up nonvolar skin, the John Hopkins team employed multiple methods, including in vitro cultures, genetic analysis, and bioprinting. Finally, they conducted a clinical trial on human volunteers, in which they took volar cells from each subject’s feet or palms, injected them into the thighs (which have nonvolar skin), and observed the resulting changes. To be more precise, they transplanted volar fibroblasts—specialized cells that reside in the dermis, just below the skin’s surface (or epidermis)—to nonvolar sites.
Cutting to the chase: The introduction of volar fibroblasts caused nonvolar skin to acquire volar traits. It did not become fully volar in their trial, the authors are careful to note: “Although fibroblast therapy does adjust tissue identity, it does not induce a large-scale and complete identity conversion” in epidermal cells. However, their study did achieve significant changes in skin firmness, epidermal thickness, gene expression, and protein composition. “These data demonstrate the distinctive properties and therapeutic potential of volar fibroblasts to modify skin identity toward a volar phenotype and greater pressure adaptation,” they conclude.
The next step, says Garza, is to test this process on actual amputees. That’s already underway: His team is recruiting amputees for a Phase 2 study where volar fibroblasts will be transplanted into residual limbs, yielding hard data on whether this therapy can lead to fewer pressure sores, blisters, and other maladies. In a very real sense, it’s where the rubber meets the road. This phase is expected to wrap up next year, and it would have to be followed by a large-scale Phase 3 study before the therapy became widely available. So we’re still several years out from anything you can request from your dermatology clinic.
But if the effort ultimately does yield an effective therapy, it could be a true game-changer for amputees. And the implications could extend far beyond the limb-loss community.
“Nobody has done cellular therapy that’s been successful in solid organs,” says Garza. “Cellular therapy works in blood cancers, for example, and people have tried blood injections into organs, such as platelet-rich plasma. There have been efforts that involved injecting stem cells into the heart. But the great thing about cell therapies involving the skin is that we can test them without a lot of risk to the patient. Cellular therapies involving the heart, the brain, or any internal organ are a lot more difficult to test. With a skin cellular therapy, we can inject the cells easily and we can monitor it very easily. If a problem arises, we can remove it pretty easily. So the skin is a great test case for cellular therapy in general.”
The full paper is available (paywalled) at science.org. Amplitude will be following this research closely as it moves forward.