Scoliosis, a complex spinal deformity, has been a focus of medical intervention for centuries. The evolution of scoliosis bracing from rudimentary beginnings to sophisticated designs reflects significant advancements in medical science and technology. This article aims to provide a concise historical overview, examine the current state of bracing technology and explore the potential future enhancements through the lens of 3D CAD design and additive manufacturing.
Hippocrates' Contributions
The genesis of scoliosis bracing can be traced back to the Father of Medicine, Hippocrates1 -4 (circa 460-370 BC), who was the first to devise a methodical approach to treating spinal deformities. Among his numerous contributions to medical science, the scamnum stands out as the earliest known orthopaedic device specifically designed for the correction of spinal curvatures. This device, a form of traction table, was ingeniously crafted to apply longitudinal force along the spine, aiming to straighten abnormal curvatures.
Hippocrates' scamnum was not only a reflection of the medical knowledge of the time but also a precursor to the concept of external bracing that would evolve over the millennia. The scamnum's design and application are well-documented in the Hippocratic corpus, providing a window into the ancient approach to spinal deformities, with Galen of Pergamum5 a student of Hippocrates, adding direct pressure to the traction in the 2nd century AD.
Renaissance Advances
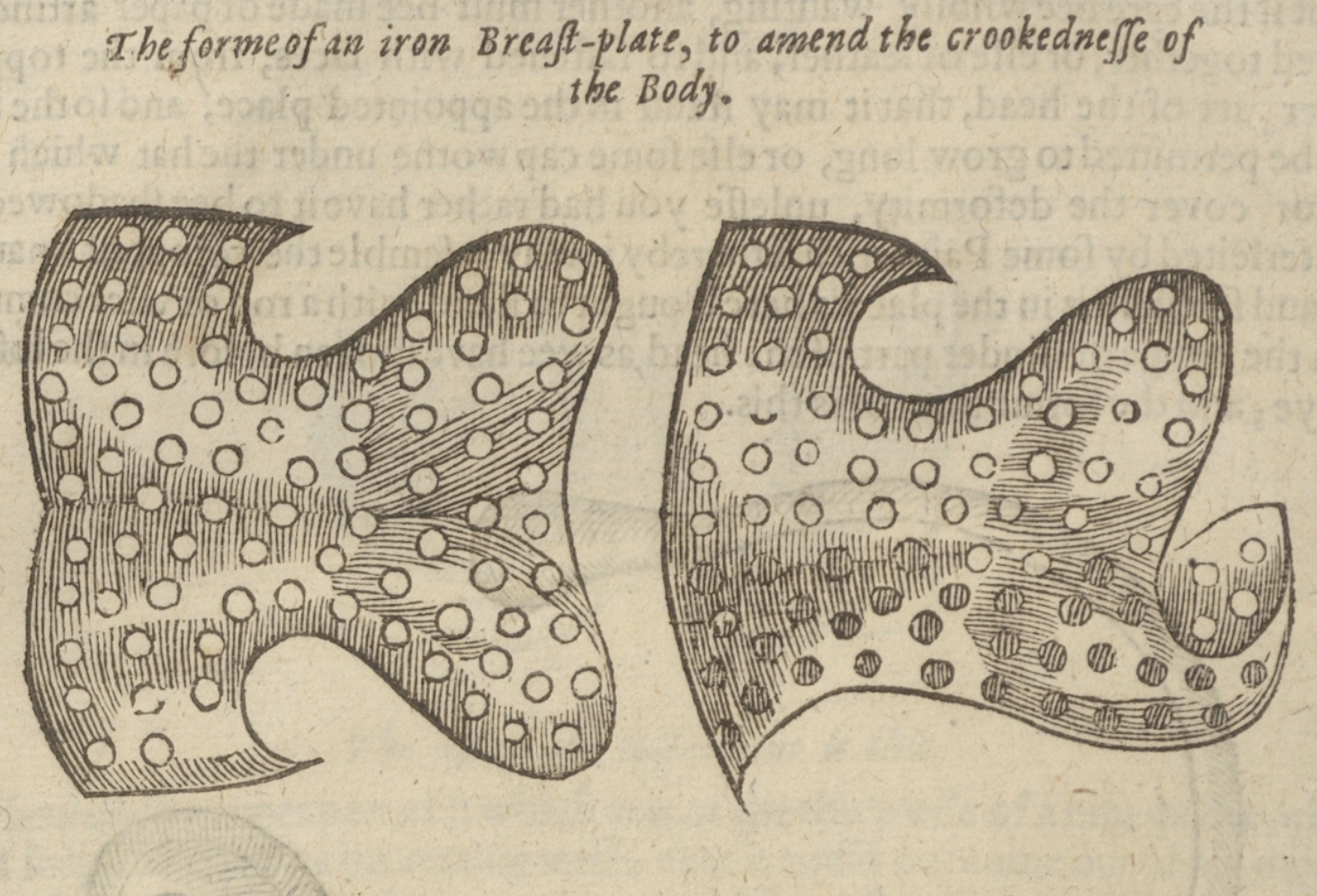
Fast forward to the Renaissance, a period marked by a resurgence of scientific inquiry and innovation, and we encounter Ambroise Pare6 (1510-1590), a French surgeon whose contributions to the field of surgery and bracing were revolutionary. Pare is often celebrated for reintroducing the principles of Hippocrates and Galen to a world where medical practices had stagnated during the Middle Ages. His work in the development of external bracing was groundbreaking. Pare designed and utilised a variety of braces and apparatuses for the correction of spinal deformities, which were more sophisticated and anatomically considerate than their predecessors.
Pare's devices were often made of metal and other rigid materials, providing external support to the spine in a manner that was more targeted and effective than the scamnum. His work laid the foundation for the understanding that bracing could be used not only to alleviate pain and discomfort but also to halt or even correct the progression of spinal deformities, with reported success! Pare's dedication to the craft of surgery and the welfare of his patients earned him the title of the father of modern surgery and his innovations in bracing set the stage for the future development of orthotic devices. Pare also noted that bracing after skeletal maturity did not provide the same results.
The lineage from Hippocrates' scamnum to Pare's braces represents a continuum of innovation and improved understanding of scoliosis treatment. These ancient foundations and progressive insights laid the groundwork for the sophisticated bracing technologies that would emerge in the centuries to follow. The commitment to enhancing patient care through innovation in bracing has remained a constant theme throughout history, reflecting the enduring legacy of these early pioneers.
The Twentieth Century: A New Era of Bracing
The 20th century heralded a transformative era in the management of scoliosis, marked by significant advancements in bracing technology. Two pivotal developments during this period, the Milwaukee brace and the Boston brace revolutionised nonoperative treatment approaches for scoliosis and remain cornerstones in the history of orthotic management of this condition.
The Milwaukee Brace
Introduced in the late 1940s by Dr. Walter P. Blount and his colleague, Albert Schmidt, the Milwaukee brace represented a paradigm shift in the conservative treatment of scoliosis. This cervicothoraco-lumbo-sacral orthosis was the first of its kind to apply corrective forces to the spine in three planes: coronal, sagittal, and transverse. The brace consisted of a pelvic girdle made from metal, a contoured metal upright, a neck ring, and anterior and posterior pressure pads strategically placed to apply corrective forces to the spinal curvature. Initially for immobilisation after surgical treatment of neuromuscular scoliosis but latterly used for the non-surgical management of Adolescent Idiopathic Scoliosis (AIS).
The Milwaukee brace's design allowed for adjustments to be made as the patient grew and as the curvature of the spine changed, providing a dynamic approach to treatment. Its introduction was a significant milestone, as it was the first brace.
The Boston Brace
The development of the Boston brace in the 1970s offered a more discreet alternative to the Milwaukee brace. Designed by John Hall and colleagues at the Boston Children's Hospital, the Boston brace, or thoraco-lumbo-sacral orthosis that could be used to treat high thoracic and thoracolumbar curves effectively. The brace's efficacy in halting curve progression and, in some cases, reducing the degree of curvature was established in the literature, with Blount and Schmidt's seminal work documenting its success and setting the stage for widespread adoption.
Despite its effectiveness, the Milwaukee brace was not without its drawbacks. The conspicuous nature of the brace, extending from the pelvis to the neck, often led to psychosocial issues, particularly in adolescents who were self-conscious about their appearance. Patient compliance was poor, mostly related to discomfort and aesthetics. Nevertheless, the Milwaukee brace remains a testament to the ingenuity of mid-20thcentury medical science and a significant step forward in scoliosis treatment. (TLSO), was a lower-profile brace that did not extend above the shoulders, making it less visible under clothing. This brace was designed to treat curves located below T8 and became the most widely used brace for the treatment of adolescent idiopathic scoliosis in the United States.
The Boston brace operates on the principle of providing symmetrical circumferential pressure to the trunk, with strategically placed pads to apply corrective forces to the spinal curvature. Its design allows for a more comfortable and cosmetically acceptable form of treatment, which has been shown to improve patient compliance. The effectiveness of the Boston brace for certain types of curves has been well-documented, with studies demonstrating its ability to prevent curve progression and, in some cases, reduce the need for surgical intervention 10.
The Boston brace marked a significant evolution in bracing philosophy, focusing on patient comfort and compliance while maintaining the corrective. The Boston brace is still widely prescribed today, however, with a symmetrical design, the primary aim of a Boston brace is to reduce further progression of a curvature rather than focus on correction. The Boston brace commonly has the straps at the rear so that the patient often needs help to don and doff the brace, which makes independent use difficult.
Furthermore, without the corrective voids of modern braces, long-term use of TLSO braces poses the risk of causing muscle wastage and potentially reducing lung capacity.
Customisation and Three-Dimensional Correction: Cheneau and Beyond
The latter part of the 20th century and the early 21st century have seen significant advancements in principles established by the Milwaukee brace. Its development reflected a growing understanding of the importance of patient-centred care in the management of scoliosis. The introduction of the Milwaukee and Boston braces in the 20th century set new standards in the non-operative treatment of scoliosis. These braces not only improved the physical outcomes for countless individuals with scoliosis but also influenced subsequent brace designs and the overall approach to conservative management of the condition. The legacy of these braces is evident in the continued innovation and refinement of scoliosis treatment strategies in the 21st century.
The field of scoliosis bracing, with a particular focus on customisation and three-dimensional correction. These developments have been driven by a deeper understanding of scoliosis as a three-dimensional deformity, necessitating a more complex and patient-specific approach to treatment.
The Cheneau Brace
Introduced in the 1970s by Dr. Jacques Cheneau, the Cheneau brace marked a significant departure from previous bracing concepts by addressing scoliosis as a three-dimensional deformity. Unlike the symmetrical pressure application of earlier braces, the Cheneau brace employs an asymmetrical design to exert targeted pressures on the rib cage, guiding the spine into a corrected position. This approach aims to not only halt curve progression but also to reduce the curvature by influencing the spine's sagittal and transverse planes. The brace's design is predicated on the principle of detorsion, and its efficacy has been supported by clinical trials, which have shown promising results in managing the pubertal growth spurt in girls with idiopathic scoliosis
The Rigo System Cheneau (RSC) Brace
The Rigo System Cheneau brace is a refinement of the original Cheneau brace, incorporating the principles of three-dimensional correction with a more individualised approach 15. Dr. Manuel Rigo, a prominent figure in the field of scoliosis treatment, has been instrumental in evolving the Cheneau brace into a system that considers the unique spinal anatomy and curve pattern of each patient. The RSC brace is designed to apply corrective pressures and de-rotational forces tailored to the patient's specific spinal curvature, promoting an active correction through the patient's movements and breathing. The brace's effectiveness is closely tied to a thorough clinical assessment and precise brace adjustment, underscoring the importance of customisation in scoliosis treatment.
The ScoliBrace
The advent of computer-aided design (CAD) and computer-aided manufacturing (CAM) technologies. has further revolutionised scoliosis bracing with the introduction of the ScoliBrace. This modern brace combines the principles of the Cheneau brace with advanced technology to create a highly customised orthosis. The ScoliBrace system utilises 3D body scans to accurately model the patient's torso, allowing for a brace design that is precisely contoured to the individual's anatomy. This level of customisation has been shown to improve clinical efficacy and patient acceptance, as the brace can be both more comfortable and more effective in managing adolescent idiopathic scoliosis.
Integration of Three-Dimensional Scanning and Printing
The integration of 3D scanning has been a significant step forward in customising braces for scoliosis patients. 3D scanning allows for the creation of a precise digital model of the patient's torso, which can then be used to design a brace that fits perfectly. This process not only enhances the comfort of the brace but also ensures that the corrective forces are applied accurately to the deformity. A study by Li et al. 17 demonstrated the feasibility of using 3D scanning and printing to create a patient-specific orthosis for managing adolescent idiopathic scoliosis. The study found that the 3D-printed orthosis was wellreceived by patients and suggested that this technology could lead to improved treatment outcomes.
However whilst 3D scans are commonly used for brace design, the manufacturing process has remained the same for decades. Once the design is finalised in CAD software a 3- dimensions model of the patients corrected torso is milled in polyethylene (PE). Then a sheet of polypropylene (PP) is heated until flexible and then vacuum formed around the milled PE torso. Once cool the plastic holds the shape of the corrected torso and post production can begin to polish the edges of the brace and add velcro straps. This process 1s labour intensive, creates a lot of waste and has many steps, therefore the cost and timescales involved are significant. It also requires high levels of technical skill from the orthotists to make sure that the brace material follows the contours of the corrected torso model, otherwise the accuracy of the brace is compromised.
Problems of Compliance
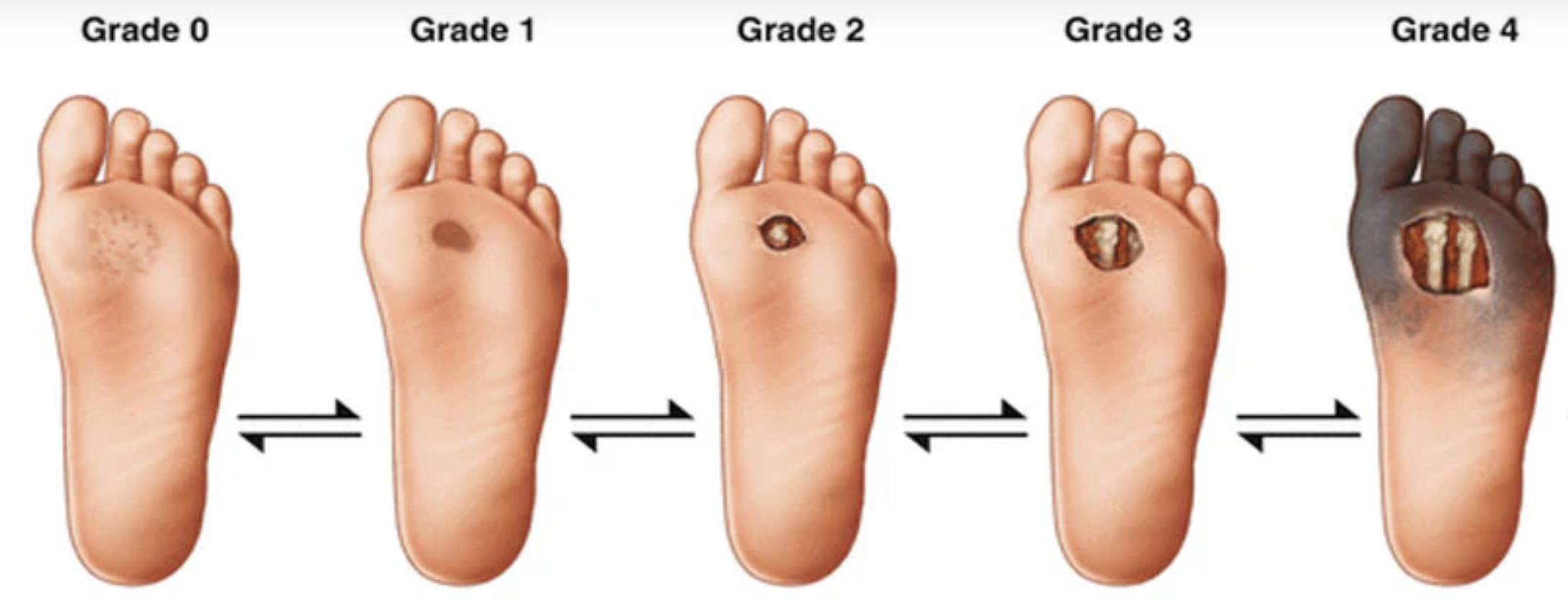
The problems a scoliosis bracing specialist faces are not solely related to the physical correction of the spinal curvature in three-dimensions, but also encompasses patient compliance, comfort, and psychosocial considerations and is well documented in the literature18-21. Traditional bracing methods, while effective to a degree, have been met with challenges related to comfort and aesthetics, particularly impacting adolescents and postmenopausal women who constitute the majority of brace wearers, although teenage boys are more frequent wearers of braces for kyphotic conditions such as Scheuermann's disease. In fact, some patients choose spinal surgery instead of a brace or corset because they do not think they can tolerate wearing a large and uncomfortable plastic brace for up to 23 hours a day for potentially many years until skeletal maturity. In fact 72% of a study population reported to be in some way psychologically affected by the brace wearing. So something must be done to improve patient compliance with the most commonly cited reasons for lack of compliance being discomfort and mental health/anaesthetics both impacting negatively on one's physical and mental well-being.
The Future of Bracing: Three Dimensional Printing
The advent of large-format 3D printers signifies a promising future for scoliosis bracing, with the potential to overcome many limitations of current bracing methods27. For years the authors have worked with top professors of additive manufacturing and composite materials and up to now they have not been able to produce a whole brace in one print and keep the costs down to something that a national health service or private paying patient could consider. The benefits of 3D printing include fast in-house production, low waste, cost reduction, weight minimisation, and extensive customisation28.
However, the market has yet to see the widespread availability of these 3D-printed braces as cost, size, strength and durability have all been limiting factors. 3D printing utilising the right materials can be sustainable with limited waste compared to the traditional vacuum forming process. It can produce braces with designs that improve airflow at the same time as reducing weight and creating a more aesthetically appealing end product that still provides the level of correction required.
Addressing the Problem: Design and Comfort
The design process for contemporary braces typically involves 3D scans and X-rays, informing the CAD designer to create the brace29. Despite technological advancements in design, the manufacturing process has remained relatively unchanged for decades, leading to common patient complaints regarding the rigidity and discomfort of solid plastic braces. Some manufactures are starting to 3D print scoliosis braces but they are using single wall PP which creates a similar product to the current vacuum forming process, but with the aded risk of fault lines created during printing. This method is slower, more costly and produces a less reliable product than traditional vacuum forming and so adoption is likely to be limited. By harnessing 3D printing to create braces that are not only corrective but also more comfortable one would hope to improve patient compliance. Moreover, by introducing variable density zones within the brace, providing flexibility in sensitive areas while maintaining corrective integrity at the curve apexes the bracing specialist can maximise correction and comfort wherever needed; and gain added strength and stability.
Variable Density Zones.
As far as the author is aware, there is only one company in the world that has managed to perfect an algorithm that can reliably vary the density of any part of the brace required by the designer. They are based in Denmark and are called Create It REAL: Their proprietary CAM slicing software and CorsetMaker large format printer allows the brace designer to apply unlimited variable densities to each design, making a truly bespoke product. The resultant brace is both firm and corrective around the apexes of the curvature whilst having lower density regions around boney prominences and known areas of discomfort, such as the iliac crest, axil la and under the breasts in females. Considering the brace is approximately 4 mm thick, the 3-D printer must create an inner and outer wall and then vary the density of the filament in the intervening cavity.
The exact design of the variable density zones is part of a patent application by Create It REAL, but we understand that it utilises a lattice structure design for strength and support in all planes. This process also reduces the risk of fault or fracture lines within the brace which occurs in single wall PP braces. This process must use a specialist 3-D printer and modern hybrid biocompatible filament materials. Initial designs took up to 36 hours to print with current production taking approximately 24 hours per brace.
Whilst Create It REAL are working on reducing print time these printers can run 24 hours a day with remote viewing capabilities, making it an attractive option for bracing centres with relatively low production needs. however, print speed will need to significantly improve before any large production centres can use this technology at scale. Nonetheless, the benefits of a variable density brace outweighs the increase print time over solid wall, polypropylene 3-D printed braces.
Addressing the Problem: Design and Aesthetics
Most brace designs focus on the clinical needs of the spine, but do little to consider the aesthetic concern of the patient who are often teenage girls. The author proposes that medical professionals should engage more with corsetiers, dressmakers and designers who understand how to flatter and make the human form beautiful. This type of collaboration may bring about a new era of design in spinal braces with increased compliance30. If a patient sees their brace as a work of art, a personalised fashion statement rather than a cumbersome medical device, the author feels that patient of all ages are more likely to wear their brace for the prescribed time each day and therefore improve their clinical outcomes. With the ability to micro design every aspect of the brace at the CAD design stage together with unlimited post production possibilities, bracing centres can truly create bespoke products that meet the patients physical and mental/emotional needs.
Design Disagreements and limitations of current production methods.
The field of scoliosis bracing is characterised by a diversity of design philosophies, even among those utilising Cheneau principles. This variation often arises from differing beliefs about the best ways to achieve correction. During the traditional manufacturing process, cost and production time remains a significant barrier, with production centres predominantly located in the USA and labour intensive multi-step production, leading to high prices and shipping costs and an average 3-4 weeks lead time for production. 3D printing presents an opportunity to create truly individualised brace designs for each patient without the constraints of a multi-step, multimaterial production process. However, some disagreement within the field is healthy to encourage innovation, variety and ultimately choice for the patient.
Conclusion
The evolution of scoliosis bracing stands at a crossroads, with 3D printing offering a pathway to more personalised, comfortable, and aesthetically appealing treatment options. By addressing the issues of comfort and aesthetics, and by reducing production time and costs, 3D printing has the potential to significantly improve patient outcomes. As the field progresses, it is imperative to continue exploring these new technologies while addressing the complications that arise to ensure the best possible patient centre care for scoliosis suffers and those with other spinal deformities.
Matthew Potts
Clinical director of the Dorsi Spinal Institute, Nottingham and Marylebone, London.