Biotensegrity and fascintegrity are terms derived from biological and fascial tensegrity, which describe the structural integrity of biological systems based on the principles of tensegrity. Biotensegrity is the broader concept; fascintegrity focuses more narrowly on the fascia itself, while also incorporating the importance of fluid dynamics within the system. For this article, I’m simply going to refer to biotensegrity, the broader framework that includes all elements of the body (bones, muscles, fascia, tendons) working in balance through tension and compression.
Tensegrity, a concept first introduced by architect and inventor Buckminster Fuller, was later adapted by Stephen M. Levin, MD, to describe living structures that stabilize themselves through a balance of tension and compression forces: biotensegrity. In living organisms, this balance allows for flexibility, strength, and adaptability. In 2021, I introduced the concept of the biotensegrity bridge (“Human-device Integration: Introducing the Biotensegrity Bridge,” The O&P EDGE, March 2021). This article dives deeper into biotensegrity and its relevance to prosthetic socket design and its effects on the wearer.
Biotensegrity and the Human Body
The human body is a dynamic, interconnected system where structures like bones, muscles, ligaments, and fascia work together to maintain stability and mobility. According to biotensegrity principles, the body’s framework is not a rigid structure but a complex tension-compression network.
Biotensegrity in the human body has three main components:
- Bones as compression springs or struts: Bones provide support by resisting compressive forces.
- Soft tissues as tension elements: Muscles, tendons, and ligaments create tension, maintaining structural integrity and facilitating movement.
- Fascia as a connecting network: Fascia links various tissues, distributing forces across the body.
These elements offer various benefits, including efficient force distribution. Biotensegrity ensures forces like gravity, muscle contractions, and external impacts are evenly distributed, reducing localized stress. The system has inherent adaptability as it adapts to changes such as posture or injury, maintaining function, and energy efficiency. Balanced tension and compression reduce the energy required for movement and support.
Adopting and following principles of biotensegrity in O&P allows allied health professionals, engineers, and designers to develop interventions that complement rather than disrupt the body’s natural mechanics.
Biotensegrity and Prosthetic Socket Design
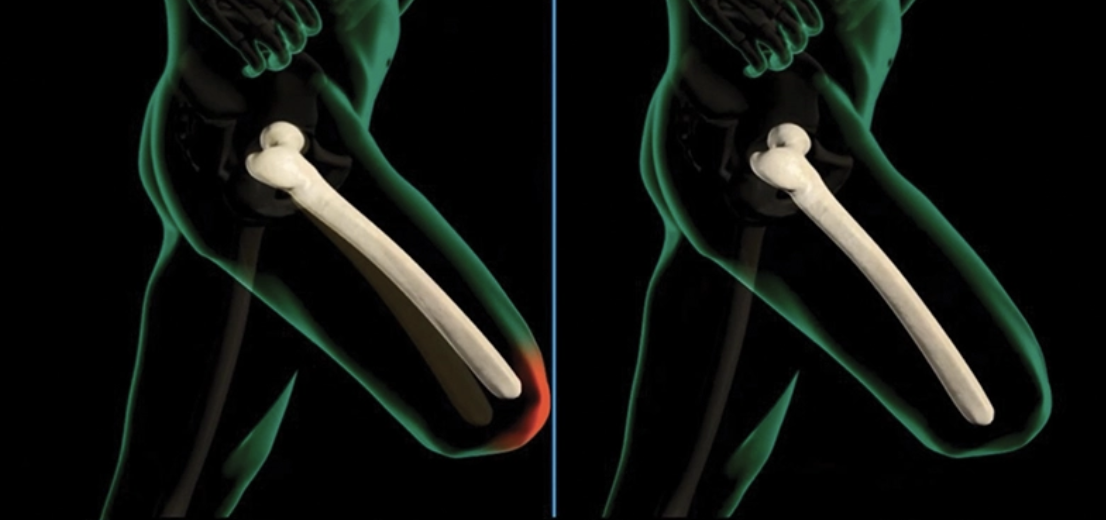
What is the goal of a prosthetic socket? There is a long list of possible answers, including, but not limited to, an attachment for downstream components, transfer of forces, stability, gait symmetry, energy savings, and comfort. But how is this accomplished? Prosthetic interfaces are perhaps most critical in the two-way transfer of forces and information between the residual limb and the prosthetic device. Traditional transfemoral socket designs and those still under development prioritize mechanical stability at midstance over respecting the body’s natural biotensegrity throughout the entire gait cycle, as well as during sitting or standing. This unidimensional prioritization often leads to discomfort, tissue breakdown, and long-term health issues as a result of the body’s attempt to compensate. Returning the wearer who has undergone a traumatic amputation to the natural state he or she was in prior to trauma should always be our goal. Simply maintaining stability at midstance at the expense of long-term health and well-being does not achieve this. While stability should always be part of the equation, it is only a base line.
Limitations of Traditional Socket Designs
Ischial containment designs are the standard of care at the transfemoral level. Because these designs mechanically and artificially support the ischial tuberosity, they provide an abrupt, vertically directed ground reaction force (GRF) at midstance, forcing the pelvis into a fixed position to stabilize the prosthesis.
The sudden and abrupt vertical GRF into the ischium at midstance can lead to negative effects on the hip musculature and overall gait mechanics in individuals with amputations, violating the principles of biotensegrity. This occurs because the socket assumes some of the support responsibilities typically allocated to the hip musculature and fascia, which can result in disuse, compensatory patterns, and long-term functional deficits.
The effects on hip musculature are threefold: muscle conditioning and atrophy, loss of neuromuscular control, and altered muscle firing patterns. When the ischial containment socket artificially supports the ischium, the hip musculature is underutilized, particularly the abductors (e.g., gluteus medius and minimus). Over time, this can lead to muscle atrophy and a decrease in strength. Reduced engagement of the hip extensors (e.g., gluteus maximus) and flexors (e.g., iliopsoas) may also occur as the socket provides extrinsic stability and limits range of motion.
Prolonged reliance on socket support diminishes proprioceptive input and neuromuscular coordination, leading to reduced control over hip movements. This can impair the person’s ability to balance and stabilize during dynamic activities.
Finally, as the socket takes over load-bearing duties, muscles may relax or reduce their contractile forces during critical gait phases. This disrupts normal firing sequences, which makes it more difficult for the individual to engage these muscles when needed (e.g., during uneven terrain or rapid directional changes) and therefore can cause excessive compensation of the contralateral limb and throughout the entire body.
Kinetic and Gait Issues
Reduced activation of the hip abductors compromises the pelvis’ ability to remain level during single-leg stance. This may cause excessive pelvic drop (Trendelenburg gait) on the contralateral side. Asymmetric loading from an overreliance on the prosthetic side for stability can lead to compensatory strategies, such as overloading the contralateral limb or excessive trunk leaning toward the prosthetic side. These compensations increase the risk of musculoskeletal pain and injury, particularly in the lumbar spine and uninvolved limb.
The lack of active engagement from the hip extensors and abductors during late stance reduces forward propulsion, leading to shorter strides and slower walking speeds, while compensatory mechanisms increase the energy cost of walking, resulting in faster fatigue and reduced overall endurance.
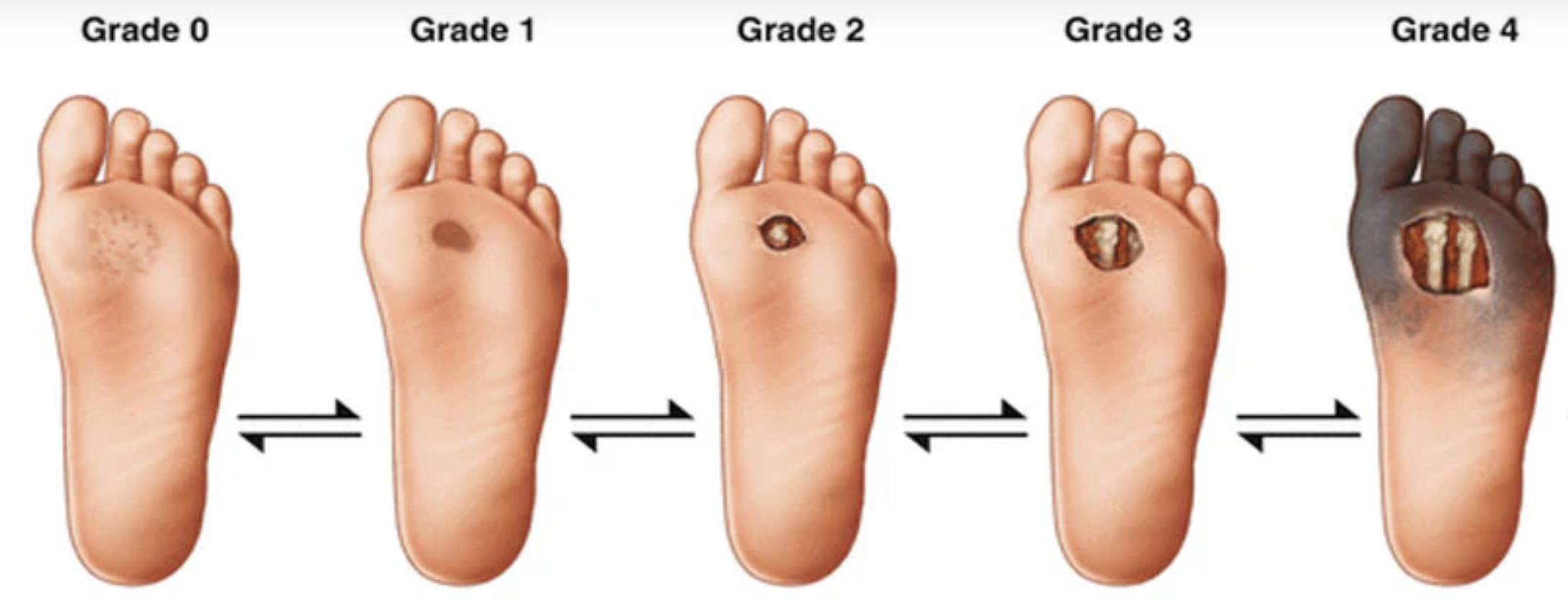
Finally, focusing primarily on midstance stability when designing a prosthetic socket, while neglecting the broader dynamics of the gait cycle, is misguided. The devotion to ischial containment at midstance while ignoring the fascia and underlying bone informs a design that completely underestimates the importance of the swing phase and its critical role in limb acceleration, deceleration, proprioception, and foot placement, as well as the other 85 or 90 percent of the stance phase wherein the ischium is not contained. This design, which extends up high into the perineum, maintains significant mediolateral pressure between a stationary or semistationary object (the ischium) and the moving femur at midstance, creating significant stress of the perineal tissues and, finally, a proximal ring of high compression.
Long-term Consequences
Chronic disuse of hip muscles can create imbalances in strength and flexibility, increasing the risk of joint dysfunction in the hips, pelvis, and lower back. When we see a long-term ischial containment wearer transition to a subischial design, lateral displacement of the interface occurs not at the interfacial boundary, where the skin meets the interface wall, but at the hip socket itself due to weakened hip musculature and its supporting structures. In addition, prolonged reliance on the socket can reinforce maladaptive gait patterns, making it difficult to achieve normal, symmetrical walking mechanics. Additionally, the inability to dynamically engage hip musculature can limit the wearer’s ability to respond swiftly and/or adequately to environmental challenges, such as slopes, stairs, or uneven surfaces, increasing the risk of falls. Finally, leaning to one side to avoid the discomfort of the raised flare of the posterior brim when sitting has long-term consequences regarding spinal alignment and soft tissue degradation.
Subischial Sockets Without Osseostabilization: A Half Measure
Subischial sockets aim to improve comfort by avoiding the ischium as a weight bearing surface. However, without an overarching focus on limiting unwanted motion of the bone within the socket, they fail to fully address biotensegrity. By allowing excessive motion of the bone, force transfer and distribution are compromised. This is akin to riding a bicycle with loose handlebars. It can be done, but it doesn’t imbue the operator with confidence, nor can it be considered altogether safe. Lack of stabilization leads to inefficient load transfer between the residual limb and prosthesis. In addition, instability increases energy expenditure during movement. While these sockets offer some improvement at the proximal brim, their benefits are limited beyond this.
Jason Kahle, MSMS, CPO/L, FAAOP, compared ischial-ramus containment sockets to vacuum-assisted suspension sockets and determined that except for medial proximal pressure, no other measures reached statistical evidence. However, all subjects preferred subischial sockets.1 Thus, subischial sockets have been found to be preferred in terms of comfort, as they avoid the ischium and have improved range of motion, but lack a functional improvement and sufficient stabilization, leading to inconsistent load transfer and potential limb instability.
Benefits of Biotensegrity in Socket Design

A biotensegrity-informed prosthetic socket mimics the body’s natural tension-compression balance, allowing for improved load distribution, enhanced mobility and comfort, and preservation of the residual limb’s health and functionality. I introduced the concept of osseostabilization via a compression-release stabilized interface over a decade ago out of my personal and patients’ frustration with current, standard-of-care sockets and their lack of function, performance, and comfort. The osseostabilized interface (now known as the High-Fidelity Interface System) was a culmination of my years of experience and aligns with the principles of biotensegrity. Its unique, patented and patents-pending compression and stabilization technology not only provides improved, omnidirectional and more natural support of the limb during the entirety of the stance phase of gait without an overly compressive proximal ring, but also enables a more accurate and supportive swing phase by more closely mimicking natural bone motion and providing fascial support when unloaded. This dynamic interaction between the prosthetic interface and the residual limb ensures better comfort, function, and health outcomes for the user.
Alternating Compression and Release: A Biotensegrity-informed Mechanism
The HiFi Interface leverages longitudinal, alternating zones of fascial compression areas around the residual limb’s fascia and underlying bone(s). This design stabilizes the bone within the prosthetic socket, allowing the limb to behave as an integral part of a dynamic tensegrity system. Unlike traditional transfemoral sockets, which rely on forceful proximal control and generalized pressure distribution downstream of the brim, the HiFi creates lightly compressive, stabilizing elements along the limb. By providing longitudinal compression elements with significant functional surface area as opposed to localized proximal pressure, adequate blood flow is ensured, and comfort enhanced.
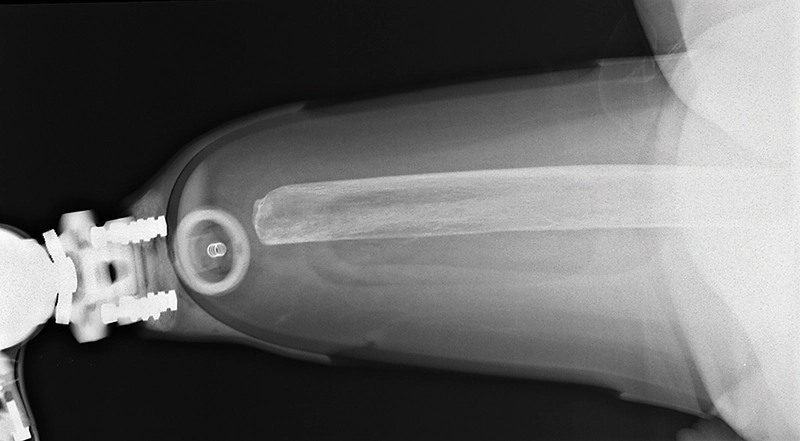
Compression zones engage specific areas around and along the shaft of the bone(s), anchoring the bone(s) and the rest of the limb securely within the socket while allowing full functional range of motion. By aligning with the body’s inherent tension-compression dynamics, the HiFi reduces localized stress while promoting efficient energy and motion transfer.
Supporting the Stance Phase
During the stance phase, the HiFi socket’s stabilization method maintains the integrity of the user’s gait by relying on fascial support, which has inherent dynamic cushioning capabilities, as opposed to ischial support. By incorporating fascial support as its primary mechanism, the hip joint musculature is allowed to return to more normal firing patterns and amplitudes. In addition, receptors in the fascia are more highly stimulated under the compression-tension relationship of the fascial support mechanism, increasing and enhancing proprioception, both in swing and stance.
The compression pattern provides improved anchoring by firming up the soft tissue at each zone, allowing the limb to support body weight without excessive translation, rotation, or slippage, and pistoning is reduced. Simultaneously, the areas of reduced compression that contribute to the alternating pattern inherent in the design, adapt to changes in tissue shape as weight shifts or loading/unloading occurs, ensuring enhanced balance as the residual limb remains securely positioned, preventing instability. Unlike ischial containment designs, the alternating compression avoids painful pressure points at the ischium or distal end, enabling prolonged wear without discomfort. And by creating a stable base, the osseostabilized interface minimizes compensatory muscle use, reducing fatigue and promoting a more natural gait.
Addressing the Swing Phase
The swing phase of gait requires precise coordination between the residual limb and the prosthetic device. Traditional sockets fail to replicate the natural movement of the bone, leading to inefficient and awkward motion patterns and reduced proprioception and kinesthetic awareness. The wearer essentially launches the socket and swings it like a pendulum, then makes a best estimate as to when to start deceleration and attempt heel strike.
Because socket position is not accurately reproduced relative to skeletal position, each stride is an exercise in speculation or guesstimation. The osseostabilized design overcomes this limitation by more accurately replicating skeletal dynamics, enabling the brain to receive proprioceptive information that more accurately reflects prosthetic orientation, condition, and position.
The alternating zones ensure omnidirectional stability and work with the residual limb’s natural motion to maintain proper alignment throughout the swing phase. This reduces the risk of gait deviations and improves overall efficiency.
Finally, by closely following the bone’s movement, and by enhancing fascial compression, the HiFi Interface provides a multitude of feedback mechanisms, surpassing even osseointegration in its scope due to its excitement of mechanoreceptors in the fascia, enabling users to feel more connected to their prosthetic limbs. This is why I have argued for years that OI in conjunction with an external, low-profile HiFi Interface is the way forward, distributing forces along the limb and away from the abutment while providing fascial compression and hence mechanoreceptor stimulation for additional feedback. Finally, soft tissue support of fascia will minimize gravitational effects on the soft tissue, preventing the significant deformation and encroachment of soft tissue around the abutment over time.
Feedback Improvement
Targeted compression can increase proprioceptive awareness by activating mechanoreceptors (like Ruffini endings, Pacinian corpuscles, Merkel cells, and Meissner corpuscles) in the fascia. Similar to what occurs in osseointegrated prostheses, osseoperception is enhanced in the osseostabilized interface, with the added benefit of heightened mechanical receptor feedback inherent in compressed fascial tissue.
This helps the user better perceive limb orientation and movement and enhances tactile and vibratory feedback from interaction with the external environment such as external impacts, uneven terrain, or contact with other surface anomalies or objects.
Perception of sustained or dynamic pressure on the limb is enhanced, as fine-tuning the interface’s compression and/or release zones can provide differential feedback, helping the user gauge limb position and contact points during movement.
Because of the targeted compression, which in turn excites the fascial mechanoreceptors, haptic feedback—a combination of tactile and force-related feedback—is enhanced, simulating force sensations more dynamically.
Over time, the nervous system adapts to interpret these mechanical signals as part of proprioceptive and tactile feedback, improving control and awareness of the prosthetic limb. A heightened compression profile and a more naturally supported and controlled limb within the prosthetic interface not only increases mechanoreceptor sensitivity and response but also reduces cognitive load on the brain, increasing the potential for embodiment. Complete prosthetic embodiment represents the ultimate integration of the prosthesis with the user’s body, mind, and daily life. It entails a seamless sense of ownership, functionality, and sensory feedback, where the prosthesis feels like a natural extension of the body rather than an external device. Achieving this state addresses multiple dimensions of user experience and quality of life.
By incorporating multiple feedback mechanisms and aligning prosthetic interface design with the principles of biotensegrity, the HiFi and future osseostabilizing interfaces can improve the overall sensory experience of the wearer and the functional performance of the prosthetic system, helping the individual achieve better control and integration of the device into their daily activities.
Conclusion
The osseostabilizing interface’s compression technology aligns prosthetic socket design with the principles of biotensegrity. By stabilizing the bone dynamically and replicating natural motion, the HiFi design supports the body’s tension-compression balance during both stance and swing phases. This improves gait efficiency and facilitates prosthetic embodiment, enhancing the overall health and well-being of prosthesis users. As a healthier alternative to traditional socket designs, osseostabilizing interfaces represent the future of prosthetic care, prioritizing function, comfort, and long-term outcomes.
Randall Alley, CP, is the CEO of biodesigns, California. He can be contacted at ralley@biodesigns.com.
References
Kahle J. T., M. J. Highsmith. 2013. Transfemoral sockets with vacuum-assisted suspension comparison of hip kinematics, socket position, contact pressure, and preference: ischial containment versus brimless. Journal of Rehabilitation Research and Development 50(9):1241-52.