As the global population continues to increase, more people are over 65, which presents unique challenges for the chiropractic profession.
These challenges provide opportunities to develop strategies for helping these people age healthier and safer. The National Institutes of Health reports that those 65 and older will soon outnumber children under age 5. There is expected to be a global increase in life expectancy, with the population of people over 85 tripling in the next 25 years. This trend creates a tremendous challenge for families caring for elderly family members. It will affect society economically, straining pension plans, health insurance and healthcare programs to support the elderly in retirement.1
The aging patient presents many complex conditions that can affect all the body’s major systems. Most of the issues that result in a patient seeking care from a DC are usually associated with joint pain of the extremities and back and neck pain, usually due to osteoarthritis.
Diabetes and cardiovascular disease are common complicating factors usually accompanied by a long list of medications. The diminishing function of the musculoskeletal system, vision, hearing and vestibular system leads to compromise and susceptibility to further pain, degeneration and injury, often leading to death.2
In 2023, more than 41,000 people 65 and older experienced falls that resulted in death. More than 68,000 fatalities were associated with traumatic brain injury. Trip-and-fall accidents are often associated with altered and diminished sensorimotor function. Our ability to respond to sources of sensory input, including visual, auditory, vestibular and proprioceptive, is insufficient to provide balance and fine motor control to navigate simple ambulation.
Falls among the elderly are significant causes of potential injuries, consequences impacting quality of life and costs to the individual and society. They are the leading cause of accidental death among the elderly. The total cost of falls among older adults in 2020 was projected to exceed $43 billion. Fifty percent of people treated in hospitals for fall injuries are discharged into nursing home care. A history of falls with no injury may induce a fear of falling, self-imposed decreased activity levels, dependence on others, social isolation, depression and reduced quality of life.3
What can be done to improve balance in our aging population?
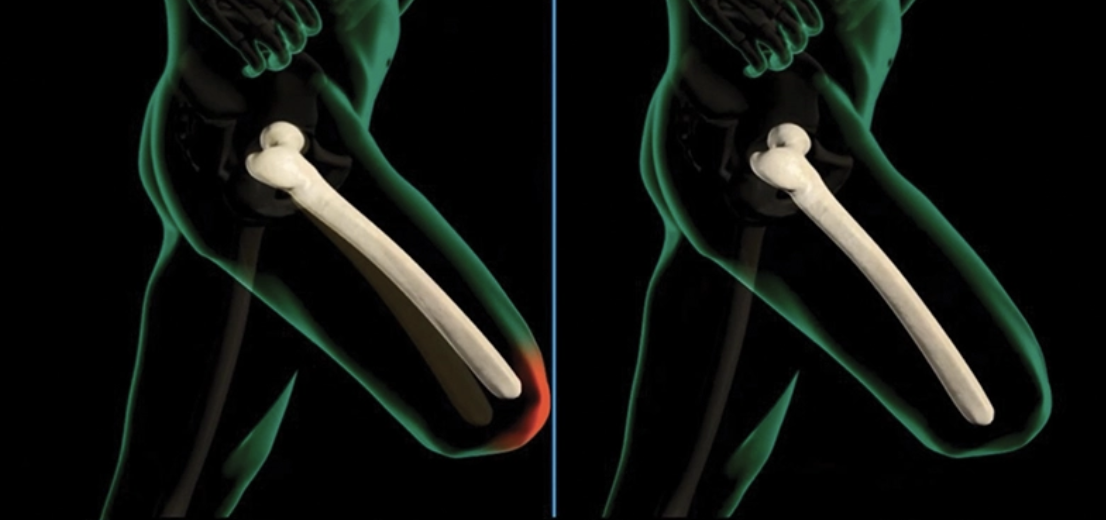
Assessment is where strategies to improve balance, posture, and functional movement are born. It’s important to look beyond symptomatic complaints and focus on the different components of structure and function. Pain complaints are often where many micro dysfunctions have accumulated to form one great compensation, a safety mechanism to limit further damage. Posture assessment is a simple way to determine how efficiently the body can bear weight and move under the influence of gravity. Forward head carriage, anterior pelvic translation and tilts of the shoulders and pelvis represent compensatory adaptations to stress, trauma, injury and anatomical asymmetries. There is a physiological limit to the body’s ability to function efficiently and these compensations create chronic stress on the tissues involved, which creates stress responses in that tissue. According to Wolfe’s and Davis’s Laws, the result is inflammation, pain and changes in the body and soft tissue structures.
ageanti-For more than 70 years, DCs have understood that evaluation of the feet is essential in determining if postural and functional movement deficits are related to foot asymmetry and biomechanical compensations related to hyperpronation. The use of custom flexible orthotics has been proven effective in reducing compensatory reflex mechanisms associated with balance. The research of Nigg and colleagues suggests that altering sensory feedback signals from the plantar surface of the foot with orthotics may allow for systematic changes in muscle activation patterns.4
In the research, altering sensory feedback signals from the plantar surface of the foot with an orthotic intervention modified sensorimotor integration mechanisms in a subject-specific manner. This indicates the feet are integral in efficient posture and balance. Good balance is neurologically unlikely with an asymmetrical pedal foundation with hyperpronation.5
A study on the effects of foot orthosis on balance in older adults provided evidence that foot orthoses could improve balance measures for older adults. Knowing poor balance is associated with risk of falls, researchers showed that the use of orthotics in screening for balance improved one-leg stance, tandem (heel-to-toe) stance, tandem (heel-to-toe) gait and alternating step tests. These tests can easily be incorporated into the initial exam to determine if the patient presents with significant balance deficits. These deficits can be addressed with custom flexible orthotics and balance-enhancing exercises.3
Balance is the primary function of the vestibular system in the inner ear and is heavily influenced by the ability of the eyes to adapt to changes in head position and posture accurately. Determining if a patient has a vestibular deficit can be challenging, but ongoing advances in understanding functional neurology have presented some simple screening methods. Learning to observe patients’ eyes and perform basic eye tracking and reflex testing can help isolate factors contributing to balance and stability deficits.
Final thoughts
In our aging patients, it is important to determine which individual components contribute to balance deficits. Posture, foot function, eye and vestibular function, flexibility, strength and fine motor control are all pieces of the balance picture. Simple interventions, including custom flexible orthotics, posture-specific exercises, stretching and appropriate chiropractic care, can make the difference between aging gracefully and a life-altering tragedy.
BRIAN JENSEN, DC, is a graduate of Palmer Chiropractic College and owner of Cave Spring Chiropractic in Roanoke, Virginia. He has been in practice for more than 35 years. As a Foot Levelers Speakers Bureau member, he travels the U.S. sharing his knowledge and insights. See continuing education seminars with Jensen and other Foot Levelers speakers at footlevelers.com/continuing-education-seminars.
References
All accessed November 4, 2024.
- Why aging matters. A global perspective. Publication No. 07-6134. March 2007. National Institute on Aging. National Institutes of Health. https://www.nia.nih.gov/sites/default/files/2017-06/WPAM.pdf.
- Older Adult Falls Data. May 9, 2024. CDC Older Adult Fall Prevention. https://www.cdc.gov/falls/data-research/index.html.
- Gross MT, et al. Effects of foot orthoses on balance in older adults. J Orthop Sports Phys Ther. 2012;42(7):649-657. PubMed. https://pubmed.ncbi.nlm.nih.gov/22282317/.
- Nurse MA, Nigg BM. The effect of changes in foot sensation on plantar pressure and muscle activity. Clin Biomech. 2001;16(9):719-727. https://pubmed.ncbi.nlm.nih.gov/11714548/.
- Burke JR. Effect of an orthotic intervention on sensorimotor integration mechanisms in patients with musculoskeletal disorders. Clinical Chiropractic. 2006;9(2):59-69. Science Direct. https://www.sciencedirect.com/science/article/abs/pii/S1479235405001008.