The devastating conflict in Gaza has created an unprecedented crisis in paediatric amputee care, with thousands of children requiring immediate and long-term support. Whilst the situation is heart-breaking, Jordan's innovative response to this humanitarian emergency could revolutionise how we care for child amputees globally, particularly in resource-limited settings.

For decades, prosthetic care has primarily focused on adults, creating significant gaps in paediatric services. Adult prosthetics are designed for stable body dimensions, whereas children's bodies are constantly growing and changing. This means children typically need multiple prosthetic adjustments and replacements throughout their development, leading to substantial ongoing social and economic costs (see www.lsngroup.org/post/early-intervention-in-prosthetic-care-the-game-changing-potential-to-unlock-higher-roi) for families and healthcare systems.
Moreover, children's prosthetic needs differ fundamentally from adults'. Whilst adult prosthetics typically optimise for work and daily living activities, children require designs that support play, school participation, and sports. Their prosthetics must be more durable to withstand active play and have different weight-to-strength ratios to accommodate their smaller frames.




The Restoring Hope Initiative in Gaza
In response to the crisis in Gaza, LSN is exploring ways of establishing a comprehensive paediatric amputee care programme that addresses these longstanding challenges through the Restoring Hope Initiative.
The approach combines several innovative elements that could serve as a model for paediatric amputee care worldwide.
The first element is the introduction of fast-fitting prosthetics, where children can be fitted with prostheses in a matter of a couple of hours, meaning that they don’t lose weeks with fittings and avoid all the commensurate complications ( physical, emotional, educational, psychological) that a delay invokes.
For upper limbs at least, fast-fitting prosthetics can be fitted within 24 hours of surgery, so the prosthesis, like getting a new pair of glasses or new shoes, immediately becomes part of their identity.
The second element is the use of modular prosthetic systems specifically designed for children, building on existing, proven technologies. The new features involve adjustable components that can "grow" with the child, significantly reducing the need for frequent replacements. The designs prioritise affordability and durability whilst maintaining functionality, making them particularly suitable for resource-limited settings. Modular prosthetics also reduce economic (and social) costs hugely (see https://www.lsngroup.org/post/transforming-lives-through-sustainable-prosthetics, as individual components can be replaced rapidly and cheaply with a child's growth.

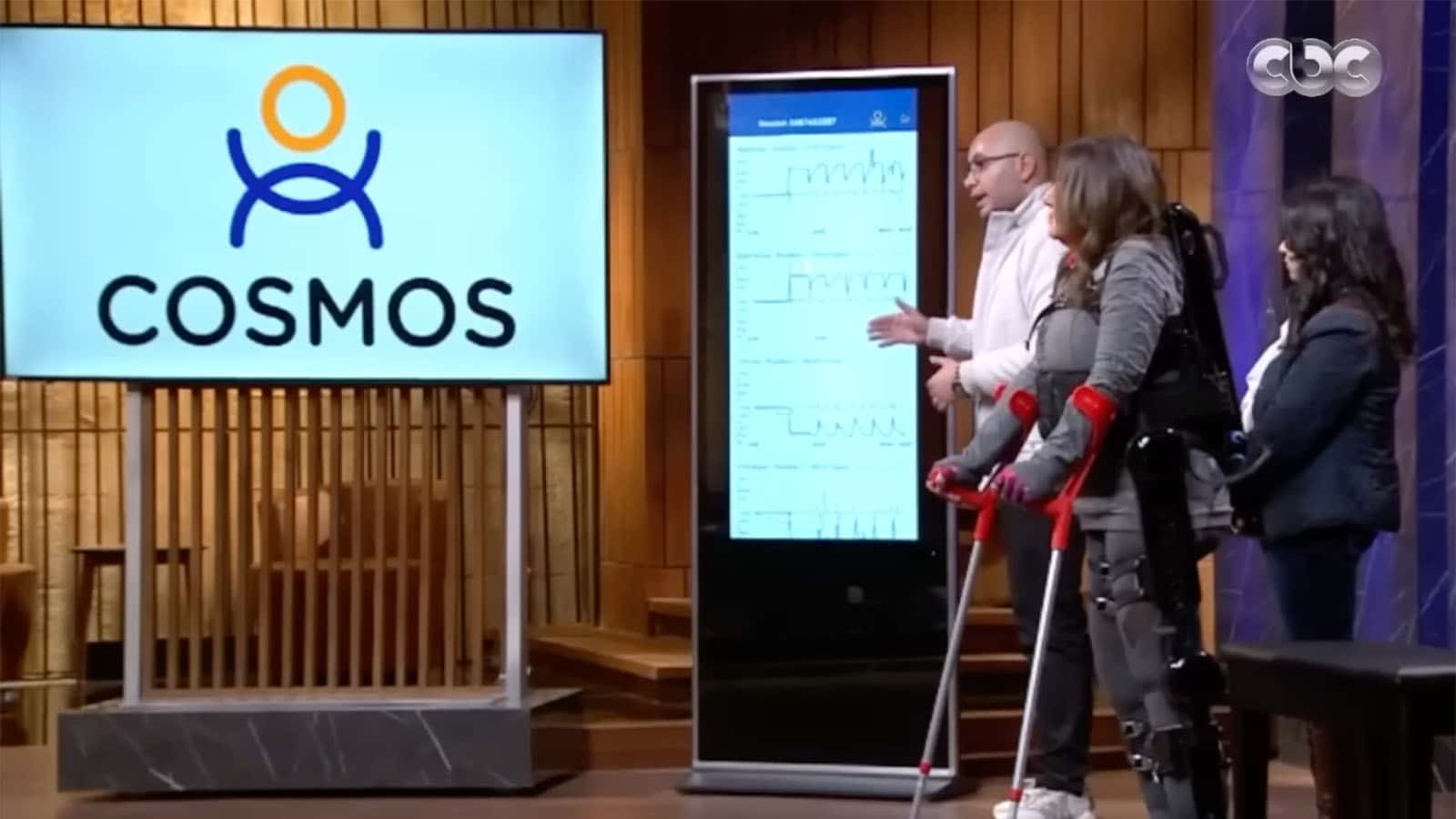
The third element is future proofing the approach so that it the amputee support services can be provided from a mobile base. A distributed care network that brings services closer to patients. Mobile prosthetic clinics can then reach children who cannot travel to major medical centres, whilst telemedicine platforms enable remote consultations and adjustments. Whilst this approach could be especially valuable in crisis situations where traditional healthcare infrastructure may be compromised, it could transform conventional thinking about healthcare infrastructures making them much more cost effective and require less capital.
Integration of Support Services
Perhaps most significantly, this new programme recognises that successful paediatric amputee care extends far beyond the prosthetic device itself. Their integrated support system needs to combine physical therapy, psychological support, and educational assistance. We have documented in other briefs peer support networks that connect families facing similar challenges, whilst vocational training programmes help older children plan for their futures.
The programme can place greater emphasis family involvement, acknowledging that children's care requires active participation from carers. Whilst in healthcare the focus is on the patient, with children the care they receive may affect the entire family. Caring for children is also about ensuring the family receive comprehensive education about prosthetic care, rehabilitation exercises, and supporting their child's psychological adjustment.
Technology as an Enabler

Modern technology plays a crucial role in making this comprehensive care model possible. New remouldable materials and 3-D printing capabilities can enable rapid, local production of prosthetic components, whilst digital health records track children's growth and adjustment needs. Mobile apps could guide families through rehabilitation exercises, and telehealth platforms maintain continuous contact between medical teams and patients.
The innovations emerging from the response to the Gaza crisis could transform paediatric amputee care worldwide. The modular prosthetic designs, distributed care networks, and integrated support systems vital in an emergency setting could address the longstanding challenges in paediatric prosthetic care that affect children everywhere, from war zones to peaceful nations.
Their model illustrates how effective paediatric amputee care must be holistic, considering not just the physical need for a prosthetic device, but the entire ecosystem of support a child needs to thrive. This includes psychological support for trauma recovery, educational assistance to maintain academic progress, and family support systems to ensure sustainable care.
Looking Forward
Whilst born from crisis, this innovative approach to paediatric amputee care offers hope for children worldwide who need prosthetic support. By demonstrating that comprehensive, child-centred care is possible even in challenging circumstances, we are creating a blueprint that could benefit children everywhere, from those affected by conflicts to those who lose limbs through accidents or illness.

As we continue to learn from this model, we have the opportunity to transform paediatric amputee care globally, ensuring that every child who needs prosthetic support receives comprehensive, age-appropriate care that supports their full development and potential. Could the lessons learned from Restoring Hope in this humanitarian crisis help establish new international standards for paediatric amputee care, creating lasting positive change from an otherwise tragic situation?