“I can’t think of anything that is more of an expression of humility than looking after someone’s feet,” says podiatric surgeon David Armstrong.
It’s a startling declaration coming from Armstrong, because if there’s any modest tender of hooves who’s entitled to a smidgen of pride, he’s the guy. A global leader in limb preservation for more than 30 years, Armstrong has helped transform the theory and practice of diabetic foot care. He has led significant innovations in the clinical, surgical, and technological domains. His work has prevented thousands of amputations and enabled people who do lose a limb to lead healthier, more functional lives.
Along the way, Armstrong has piled up lofty medical and scientific accolades that unheralded foot docs almost never receive: fellow in the Royal College of Physicians and Surgeons, visiting professorships on four continents, first podiatrist to gain admittance to the Society of Vascular Surgeons, top honors from the Association for Clinical and Translational Science…we could keep going.
Later this year, Armstrong will host the 25th iteration of the global Diabetic Foot Conference (DFCon), which he cofounded in 2001. We asked him to reflect on the last quarter-century of progress in limb care and to look ahead at the next decade or two. Here are some takeaways.
Function over form
“We believe we can eliminate preventable amputations over this next generation,” Armstrong says. “But more important than keeping your limb is keeping your mobility and independence. That transcends limb preservation. It’s functional limb preservation that’s going to matter. We’re not going to fix anyone. I think that’s the height of hubris. Our goal is to help people move through their world a little bit better.”
Toe and flow is the way to go
Multidisciplinary limb-preservation teams are becoming more common, says Armstrong. The ideal team is built around the “toe and flow” model, with a podiatric surgeon and vascular surgeon as the core players and other specialists—cardiologists, endocrinologists, physical therapists, prosthetists, plastic surgeons, and so forth—shuttling in and out of the lineup as needed. “Toe and flow supports patients all the way from being diagnosed with diabetes to getting an amputation and beyond,” Armstrong says. “We’re seeing very strong data that when you put these teams together, there’s a big reduction in high-level amputations and more limb-sparing amputations and reconstructive procedures.”
Smarter shoes and socks
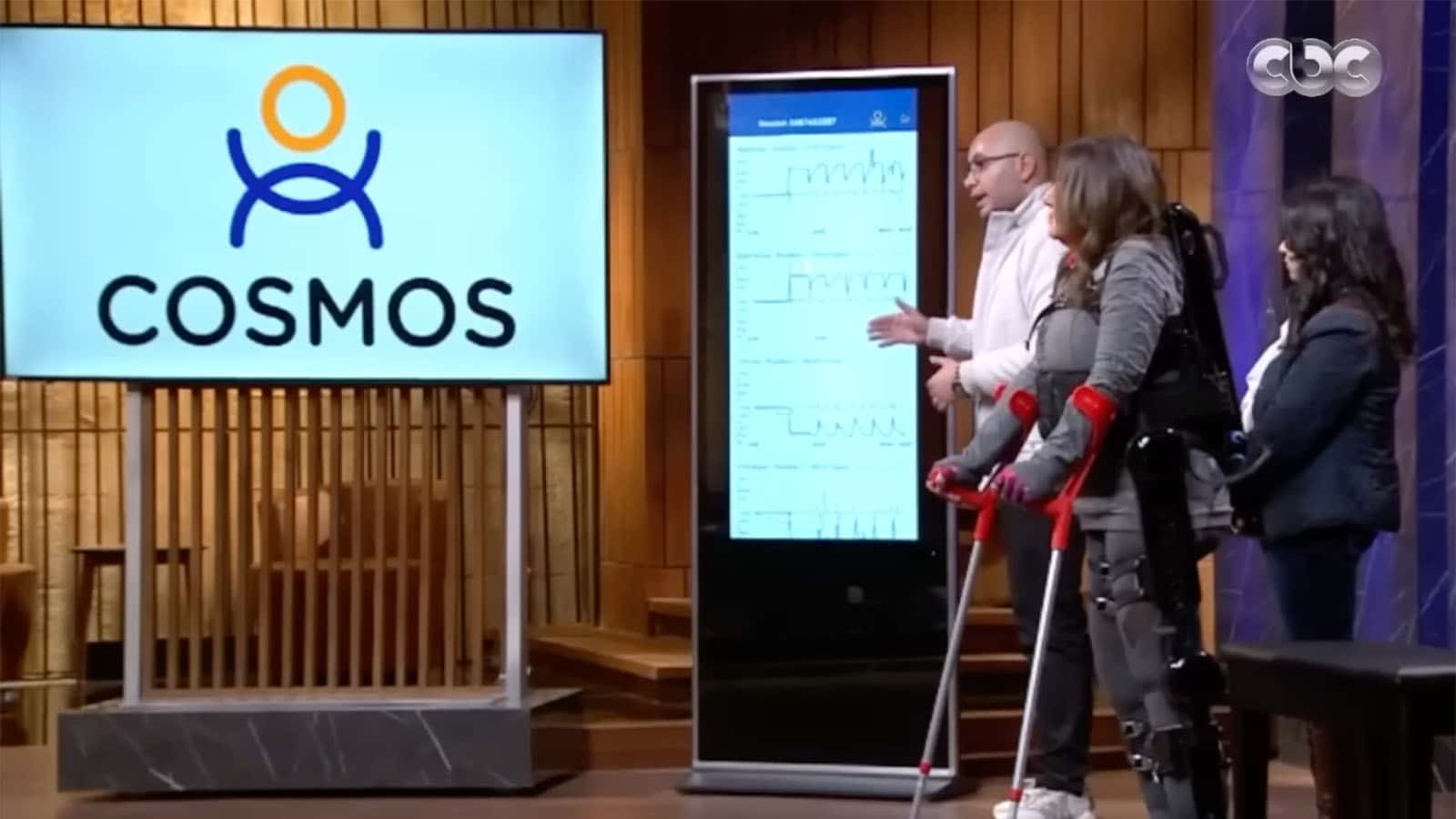
Armstrong was stunned to get a speaking invite at the high-profile Consumer Electronics Show a few years back. “I’m a toe doctor,” he laughs. “But it’s becoming geek-tastic.” He rattles off a list of startups (including Siren, SensArs, and Podimetrics) that have drawn millions in venture capital for innovative foot-preserving technologies. “There’s really cool stuff going on in neuro-modulation, in splenic stimulation, just weird things that almost make you laugh,” he says. “We envisage a time where there will be sensors on us and in us” to make foot care more responsive and more effective.
Restoring the gift of pain
“Folks with neuropathy don’t act like other patients,” Armstrong explains. “When you take away that painful feedback, then foot problems understandably become number 11 on everyone’s list of ten biggest priorities.” New sensory substitution strategies, from low-tech “foot selfies” to AI-driven circulation monitors, are emerging to refocus patients’ attention on foot health. “If we can just bump that up a little bit—if we can just make it ninth on the top ten list—then we can eliminate a lot of amputations.”